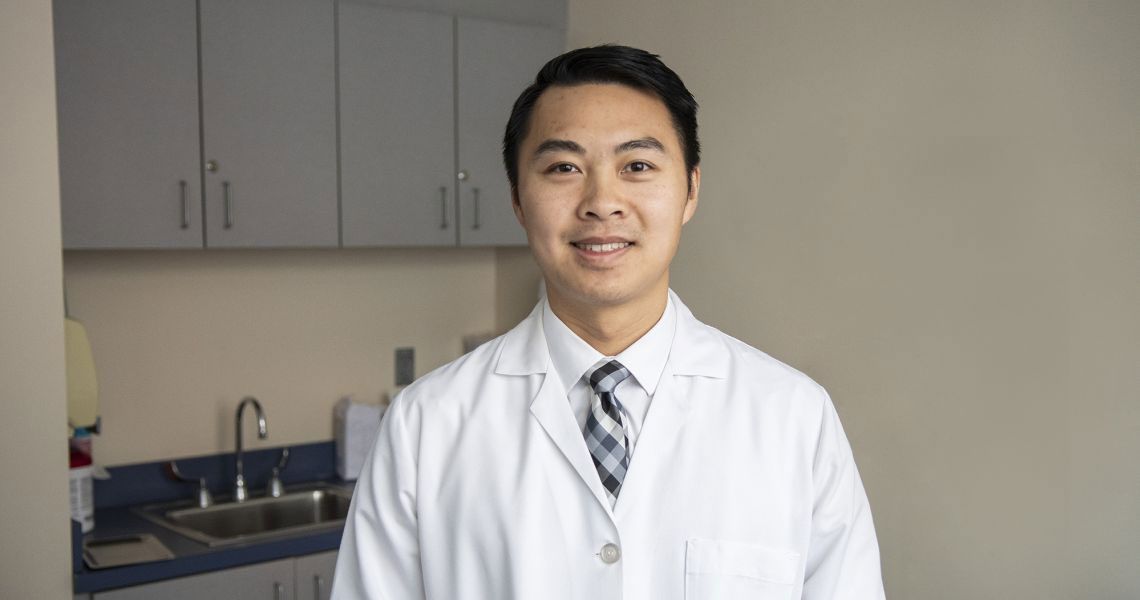
Among the cancer screenings you should regularly get after age 40, colorectal cancer, a stealthy disease that can have zero symptoms in its early stages, is one of the most important. With March as Colorectal Cancer Awareness Month, now is the time to learn more about colorectal cancer, available screening options, and potential post-diagnosis treatment plans. Matthew Ng, MD, assistant clinical professor of surgery at the George Washington University (GW) Medical Faculty Associates (MFA), walks us through the basics of the disease and what to expect from colonoscopies.
What is colorectal cancer, and how common is it?
Ng: Colorectal cancer is a cancer that originates in the large intestine (colon) or the rectum. Colorectal is a short way of saying colon and rectum. In the United States, the overall risk of colorectal cancer in average-risk individuals is about 4%. The incidence is approximately 25% higher in males than in females and 20% higher in Black Americans than white Americans.
Colorectal cancer is uncommon before age 40, with incidence increasing between ages 40 and 50. Recent data in the United States show that the age of diagnosis is increasing in the 40-50 population and decreasing in older groups.
What are symptoms of colorectal cancer?
Ng: A majority of patients with colorectal cancer are symptom-free, which is why screening is so important. This is to identify early-stage cancer before it becomes symptomatic and potentially harder to treat. Early-stage cancer is rarely symptomatic.
As the cancer progresses, symptoms including passage of blood through the anus, usually with or in the stool, abdominal pain, unexplained iron deficiency anemia, change in bowel habits, and unintentional weight loss all can be present. Less common symptoms include abdominal distension, nausea, or vomiting, which can be signs of a blockage.
What are polyps?
Ng: A polyp of the colon and rectum refers to an abnormal growth of the lining of the colon and rectum that grow into the lumen [the opening inside the colon and rectum]. They are usually asymptomatic, but sometimes they can cause bleeding or pain if located in the rectum. When they get very large, they can cause intestinal blockage. Some polyps can turn into cancers, but a majority are benign when found.
How do you diagnose colorectal cancer?
Ng: Colorectal cancer is normally diagnosed with a colonoscopy. A colonoscopy is a flexible camera that is inserted through the anus, and it allows for the entire inside lining of the colon to be evaluated. If something abnormal or suspicious is found, a biopsy is performed, where a piece of the lining is removed and examined under a microscope.
What should patients know about getting a colonoscopy?
Ng: There are many misconceptions about a colonoscopy. A colonoscopy is the best way to detect colorectal cancer. It is an outpatient procedure and is fairly quick (less than one hour). The patient will be sedated so they will not feel anything. To have a successful colonoscopy, the patient must drink bowel prep, a solution that will clean out the bowels so that we can see the inside.
There are stool tests advertised for colorectal cancer screening. These are only recommended for patients that are average risk for colorectal cancer. That being said, if a patient is having the above symptoms or a family or personal history of polyps or cancer that puts them at high risk, these stool tests are not meant for screening.
What do treatments involve?
Ng: When someone is diagnosed with colorectal cancer, the first step is to determine the stage of the cancer. Staging involves figuring out how involved the cancer is, including whether there are [affected] lymph nodes or if it has spread to other organs. We then develop a unique treatment strategy for each patient. This plan includes, but is not limited to, surgery to remove the affected area and chemotherapy and/or radiation therapy before or after the cancer is removed.
How can patients prevent colorectal cancer from developing?
Ng: The best way to prevent colorectal cancer from developing is to get screened and maintain screening. Polyps can turn into cancer. If polyps are found and removed, we can prevent colorectal cancer from growing. Other factors, shown in some studies, that can be associated with a decreased risk in colorectal cancer include regular physical activity, consuming a fiber-rich diet high in fruits and vegetables, and regular use of aspirin or NSAIDs [such as ibuprofen].
How does the GW MFA care for patients with colorectal cancer?
Ng: Patients diagnosed with colorectal cancer are automatically placed into the cancer network. The patient is treated by a multidisciplinary team of physicians that includes radiologists, oncologists, radiation oncologists, colorectal surgeons, gastroenterologists, and pathology specialists. Our nurse navigator will help guide the patient along the way. This guidance includes setting up the appointments for surgery and chemotherapy and radiation therapy. After the patient has recovered from cancer, there are support groups for survivors as well as genetic counselors. Treatment does not stop once the cancer is removed; the patient will continue their care with our team to ensure that it does not come back.
To make an appointment with a colorectal surgeon, visit the Center for Colon & Rectal Surgery at the GW MFA or call 202-741-3243.