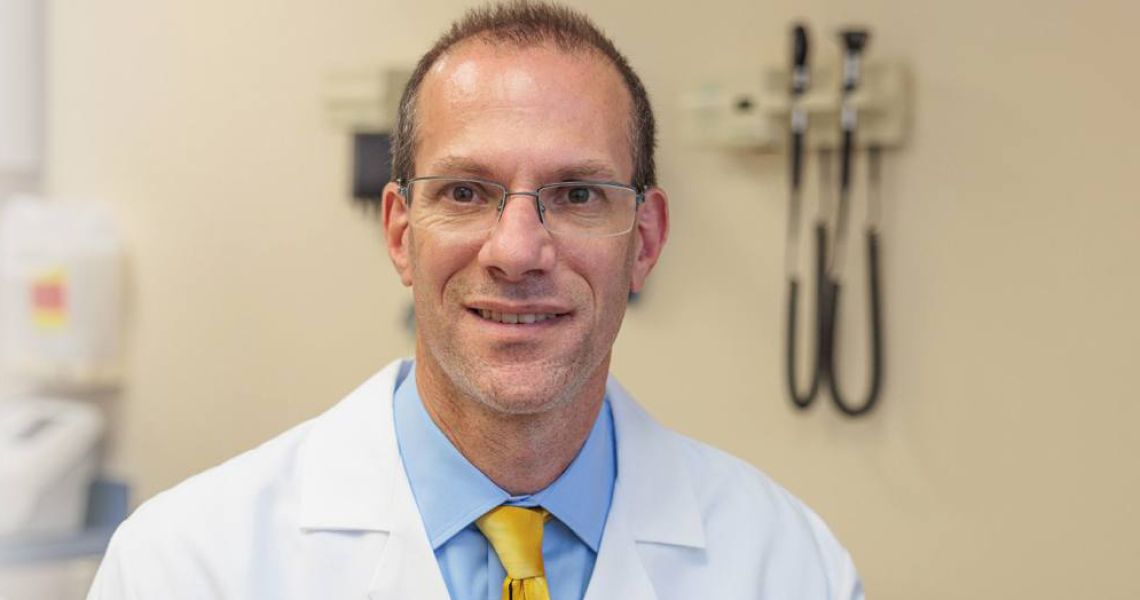
Whether you suffer from persistent knee pain and stiffness, or you’ve suffered a knee injury, knee replacement surgery may be in your future. Billed as one of the most successful surgeries, according to the American Academy of Orthopaedic Surgeons, these procedures can have an indelible impact on your quality of life. Here, Robert Sterling, MD, chair of the Department of Orthopaedic Surgery at the George Washington University (GW) School of Medicine and Health Sciences (SMHS), explains the basics of the surgery, who qualifies, and what to expect from surgery and recovery.
What health conditions or injuries can lead to knee replacement surgery?
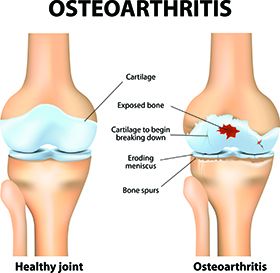
Sterling: The vast majority of knee replacement surgeries performed around the world are due to osteoarthritis or what is commonly called “wear-and-tear” arthritis. Over a lifetime of knee use, the ultra-smooth surface of the joint (the cartilage) can become worn away, making the joint no longer move smoothly. As the surface wears down over time, the knee can become increasingly stiff and painful, which are the two most common symptoms of osteoarthritis. Other conditions that can lead to knee replacement surgery include fractures into the knee joint, osteonecrosis (also called avascular necrosis, where some of the bone cells under the cartilage die and cause the cartilage on top of this bone to collapse), and injuries to the meniscus or knee ligaments that are often associated with injuries to the cartilage or can lead to instability of the knee.
At what point is this surgery necessary?
Sterling: At this time, there is no means to reverse osteoarthritis, and treatment is directed at controlling pain and preventing loss of range of motion. The first treatments for knee arthritis generally involve participation in an exercise program to strengthen the muscles, use of a support sleeve or sometime bracing, use of Tylenol or anti-inflammatory medications, and, for appropriate patients, weight-loss programs. Many patients will also undergo treatment with injections of steroid medications (such as cortisone) or gel injections to try to control symptoms. Surgery is necessary when someone’s pain and limited motion are no longer acceptably managed by nonsurgical treatments and the patient wants to have an operation to improve the pain.
What happens during the surgery?
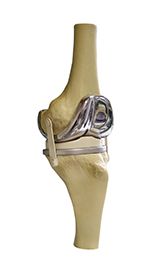
Sterling: During the surgery, the patient is brought to the operating room and given an anesthetic. The joint is opened, and the damaged cartilage surfaces are removed by cutting the bones just beneath the level of any remaining cartilage. The bones are measured to pick the proper size of replacement implant. Generally, a metal implant is placed to cover the top of the tibia (shin bone) and bottom of the femur (thigh bone). The implants are usually held in place with “bone cement,” which locks the implant to the bone. Newer technology, however, enables us use implants that are made for the patient’s own bone to grow into the implant to hold it in place. A piece of medical plastic is then attached to the tibial implant. This plastic moves beneath the implant on the thigh to recreate the smooth movement of the knee joint. During the operation, the kneecap (patella) can also be resurfaced by cutting the undersurface of the bone flat and attaching a plastic piece to the patella. Doing so allows the patella to move smoothly against the new femoral implant if the cartilage on the patella has worn away.
How long does recovery take?
Sterling: After surgery, most patients are able to start walking in the recovery room with the use of a walker. Doing an exercise program to regain strength and movement in the knee is a very important part of the recovery. Most patients will use the walker for 1 to 3 weeks, then a cane for an additional 3 to 6 weeks, and participate in an active recovery program (usually a combination of physical therapy and a home exercise program) for about three months. Patients with jobs involving mostly sitting can often return to work between eight and 10 weeks. Those with more active jobs that involve more moving about are often out of work for three months. Overall, patients will continue to make improvement in strength and endurance for many months after the initial recovery period. I generally tell patients that to see all of the benefits of surgery, their recovery will not be fully complete for about one year.
How long does a replacement last?
Sterling: For many patients, their knee replacement can last them the rest of their life. When looking at the data that has been reported on knee replacements, approximately 95% of knee replacements are still in place 15 years after the surgery, and 92% are still in place 20 years later.
How can the GW MFA help those who might need a knee replacement?
Sterling: There are several ways for patients who are ready for a knee replacement to be evaluated at the GW MFA. Patients can schedule an appointment through gwdocs.com, through their MyChart portal, by calling 202-741-3300, or emailing us at: orthopaedics [at] mfa [dot] gwu [dot] edu (orthopaedics[at]mfa[dot]gwu[dot]edu).