This page will teach you about Type 2 Diabetes and how it can be prevented and treated with a healthy lifestyle.
What Is Diabetes?
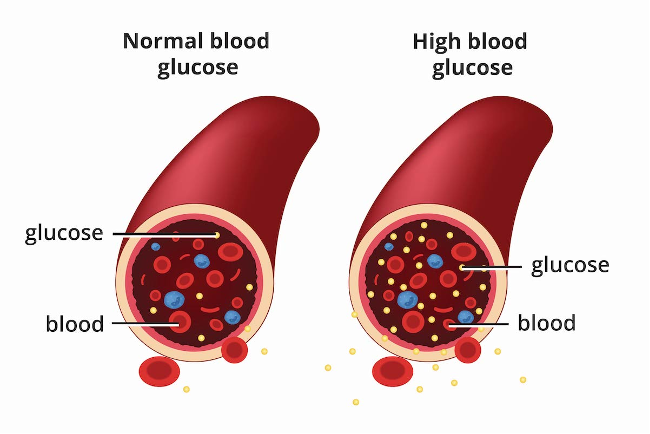
Diabetes mellitus is a condition where the body has trouble keeping blood sugar (glucose) at a healthy level. This can happen because the pancreas does not make enough insulin, because the body does not use insulin well (insulin resistance), or both. Glucose comes from the food we eat and is the body’s main source of energy. Insulin is the hormone that works like a “key,” helping glucose move out of the blood and into cells so it can be used for energy. Muscles are especially important in this process, since they are one of the main organs that help regulate blood sugar. When diabetes is not controlled, glucose builds up in the blood and can cause health problems over time.
-Shankar PS, Jali MV. Standards of Care in Diabetes-2025. RGUHS Journal of Medical Sciences. 2025;15(1)
-DeFronzo RA, Tripathy D. Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes care. 2009 Nov;32(Suppl 2):S157.
Source:
There are two main types of diabetes:
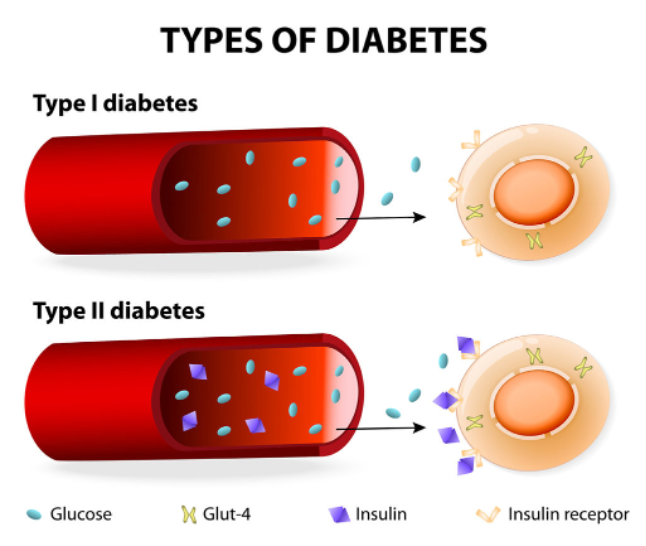
Type 1 diabetes happens when the body’s immune system mistakenly attacks and destroys the cells in the pancreas that make insulin. Without insulin, the body cannot move sugar (glucose) from the blood into the cells. People with type 1 diabetes must take insulin every day to survive.
Source: https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/type-1-diabetes
Type 2 diabetes is the most common type. In this form, the body still makes insulin, but it does not work properly (insulin resistance). Extra fat in the blood can build up inside muscle and liver cells, blocking insulin from doing its job. This causes blood sugar levels to rise. As a result, the body needs to release more and more insulin to keep blood sugar under control. Over time, the pancreas may not be able to continue to make enough insulin to keep blood sugar normal. Early on, insulin resistance and type 2 diabetes are reversible.
Source: https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/type-2-diabetes
Insulin Resistance
One of the main causes of Insulin Resistance is the toxic effects of saturated fat on cells of the pancreas, muscle and liver. The key to reversing insulin resistance is reducing dietary saturated fat.
Watch a video that explains insulin resistance in Type 2 Diabetes and Prediabetes
Clinician Notes:
Two main types:
- Type 1 diabetes = autoimmune destruction of β-cells → absolute insulin deficiency.
- Type 2 diabetes = insulin resistance + relative insulin deficiency (90–95% of cases)
Pathophysiology:
Skeletal muscle insulin resistance is considered the primary defect in T2D.
Ectopic fat in muscle and liver impairs insulin signaling and worsens hyperglycemia (Shulman, 2014).
Epidemiology: ~37 million Americans (11%) have diabetes; 90–95% are type 2.
Diagnosis: ADA 2025 criteria: A1C ≥ 6.5%; FPG ≥ 126 mg/dL; 2-hr OGTT ≥ 200 mg/dL.
Sources:
- Shankar PS, Jali MV. Standards of Care in Diabetes-2025. RGUHS Journal of Medical Sciences. 2025;15(1)
- Shulman GI. Ectopic fat in insulin resistance, dyslipidemia, and cardiometabolic disease. New England Journal of Medicine. 2014 Sep 18;371(12):1131-41.
- DeFronzo RA, Tripathy D. Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes care. 2009 Nov;32(Suppl 2):S157.
Why Should I Care About Type 2 Diabetes?
Type 2 diabetes is one of the most common health conditions in the United States, affecting about 37 million people, nearly 1 in 10 Americans, and the numbers continue to rise. Most cases (90–95%) are type 2 diabetes, which is strongly linked to lifestyle factors such as weight, nutrition, and physical activity. The encouraging news is that type 2 diabetes is often preventable with healthy lifestyle choices. For those who already have the condition, making changes in diet, physical activity, stress management, and sleep can dramatically improve blood sugar control. In fact, many people are able to reach diabetes remission—meaning their A1C stays below 6.5% for at least three months without medications—through sustained lifestyle change. Without proper management, diabetes can quietly cause complications such as heart disease, kidney failure, vision loss, and nerve damage, but with treatment and healthy habits, these risks can be greatly reduced.
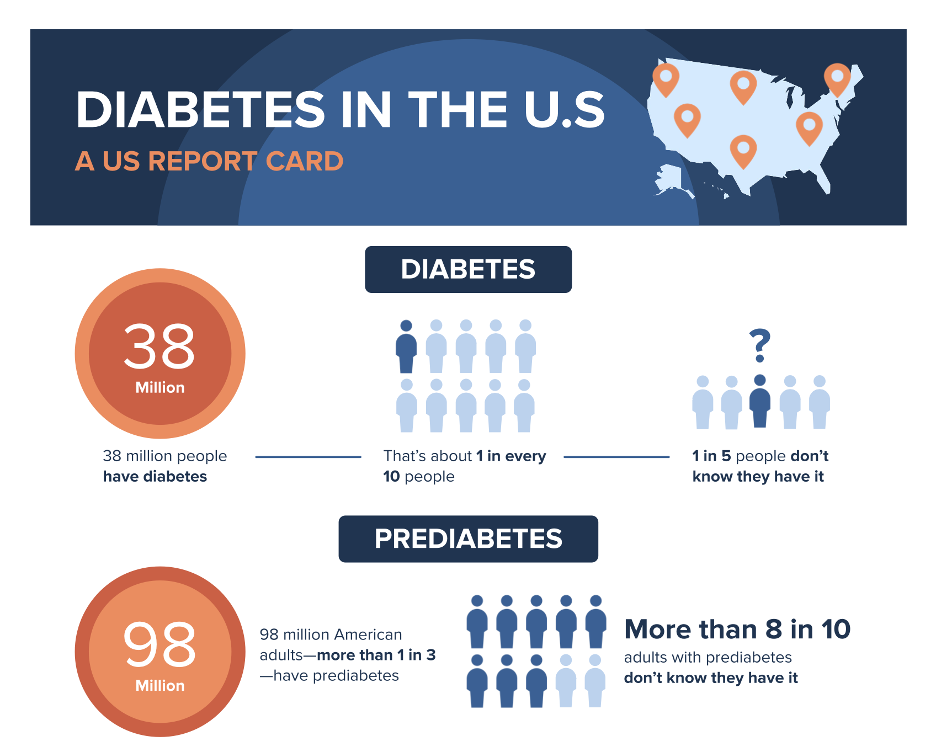


Image Sources:
How Is Diabetes Harmful to My Body?
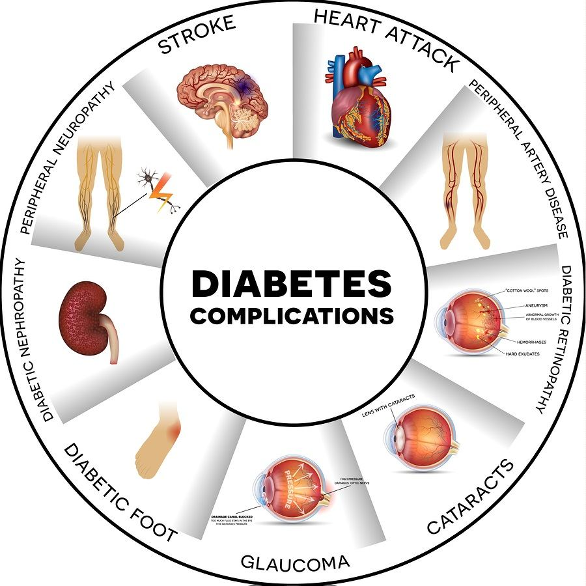
When blood sugar stays high for a long time, it damages blood vessels and nerves throughout the body. This increases the risk of many serious health problems, including:
- Heart attack and stroke – Diabetes greatly increases the risk of cardiovascular disease, which is the leading cause of death in people with diabetes.
- Kidney disease and dialysis – High blood sugar over time damages the kidneys, sometimes leading to kidney failure that requires dialysis or a transplant.
- Vision loss and blindness – Diabetes is the most common cause of adult blindness in the United States.
- Nerve damage (neuropathy) – This can cause pain, numbness, and weakness, especially in the feet and legs.
- Foot ulcers and amputations – Poor circulation and nerve damage together raise the risk of wounds that don’t heal, sometimes leading to serious infections and amputation.
Beyond these complications, diabetes can also affect your skin, digestion, sexual health, and hearing. Without treatment, diabetes can shorten life expectancy and reduce quality of life.
The good news is that with treatment — especially healthy lifestyle choices like eating well, avoiding saturated fat, staying active, managing stress, and getting enough sleep — many people are able to control their diabetes and lower their risk of complications. In some cases, people who make and sustain major lifestyle changes can even achieve diabetes remission, meaning blood sugar levels return to normal without the need for medications.
Clinician Notes:
Epidemiology: ~37.3 million people in the U.S. have diabetes (11.3% of population); 90–95% are type 2 (CDC, 2022).
Burden of disease:
2/3 of people with diabetes die of cardiovascular disease
Diabetes is the leading cause of kidney failure, blindness, and non-traumatic amputations in adults.
Prevention & remission:
Diabetes Prevention Program (DPP): Lifestyle intervention reduced diabetes incidence by 58% compared with placebo.
Remission data: Intensive lifestyle changes and weight loss (10–15% body weight) can lead to remission in up to 46% of people with type 2 diabetes.
Plain Language Summary: Lifestyle Interventions for Treatment and Remission of Type 2 Diabetes and Prediabetes in Adults
Rosenfeld RM, Donnell L, Noe DR, Levine Reisner LS, Karlsen MC. Plain Language Summary: Lifestyle Interventions for Treatment and Remission of Type 2 Diabetes and Prediabetes in Adults. American Journal of Lifestyle Medicine. 2025;19(2_suppl):155S-177S. doi:10.1177/15598276251325517
Sources:
- Shankar PS, Jali MV. Standards of Care in Diabetes-2025. RGUHS Journal of Medical Sciences. 2025;15(1).
- https://www.cdc.gov/diabetes/php/data-research/index.html
- https://my.clevelandclinic.org/health/diseases/21501-type-2-diabetes
- https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/symptoms-causes/syc-20351193
How Do I Know If I Have It?
One of the tricky things about type 2 diabetes is that many people have it for years without knowing it, because there may be no symptoms at first. When symptoms do appear, they can include feeling very thirsty or hungry, urinating more often than usual (especially at night), feeling unusually tired, having blurred vision, or noticing that cuts and wounds heal slowly. Some people also notice tingling or numbness in their hands and feet.
Because the symptoms can be subtle, the only reliable way to know if you have diabetes is through simple blood tests:
- A1C test – shows your average blood sugar over the last 2–3 months. Diabetes is diagnosed if the result is 6.5% or higher.
- Fasting glucose test – measures your blood sugar after not eating overnight. Diabetes is diagnosed if the level is 126 mg/dL or higher.
- Oral glucose tolerance test (OGTT) – measures your blood sugar before and after drinking a sugary drink. Diabetes is diagnosed if your 2-hour blood sugar is 200 mg/dL or higher.
Early detection is important, because starting lifestyle changes and treatment right away can prevent complications and may even put the disease into remission.

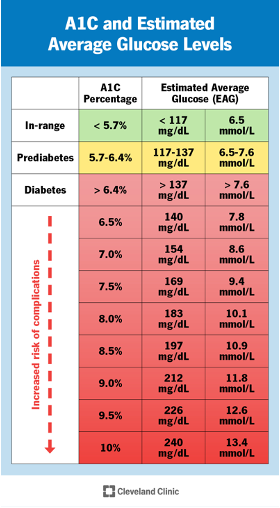
Understanding Your A1C
The A1C test is one of the most common ways doctors check for diabetes. It shows your average blood sugar over the past 2–3 months, not just a single day. That means it is not affected by what you ate the night before or by short-term changes. An A1C below 5.7% is considered normal, 5.7–6.4% means prediabetes, and 6.5% or higher means diabetes. The chart above also shows how A1C relates to your estimated average glucose (EAG), so you can see what your numbers mean in terms of daily blood sugar. The higher the A1C, the greater the risk of complications over time.
Screening for Diabetes
- Adults should start diabetes screening at age 35.
- Start earlier if overweight and you have risk factors such as:
- Family history of diabetes
- History of gestational diabetes (GDM)
- Polycystic ovary syndrome (PCOS)
- Higher-risk ethnicity (African American, Hispanic/Latino, Native American, Asian American, Pacific Islander)
- Screening is done with simple blood tests (A1C, fasting glucose, or OGTT).
| Test | Diabetes | Prediabetes | Normal |
| A1C | ≥ 6.5% | 5.7-6.4% | < 5.7% |
| Fasting Plasma Glucose (FPG) | ≥ 126 mg/dL | 100-125 mg/dL | < 100 mg/dL |
| 2-hr OGTT (75g glucose) | ≥ 200 mg/dL | 140-199 mg/dL | < 140 mg/dL |
| Random Glucose (with classic symptoms) | ≥ 200 mg/dL | - | - |
Sources:
- Shankar PS, Jali MV. Standards of Care in Diabetes-2025. RGUHS Journal of Medical Sciences. 2025;15(1).
- https://www.cdc.gov/diabetes/diabetes-testing/index.html
- https://www.fda.gov/consumers/health-education-resources/diabetes
- https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21501-type-2-diabetes
How Can a Healthy Lifestyle Prevent and Treat Diabetes?
A healthy lifestyle can lower blood sugar, improve health, and even reverse diabetes in some people. These six areas (“pillars”) are key:
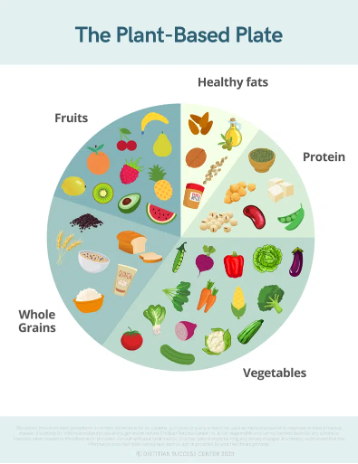
Healthy Eating for Diabetes Prevention and Management
Eating well is one of the most powerful ways to prevent and manage type 2 diabetes. A healthy diet emphasizes vegetables, fruits, whole grains, beans, nuts, seeds, fish, and healthy plant oils such as olive oil. The best plan is one that fits your cultural, religious, and personal preferences so you can follow it long term. The goal is not a “quick fix” diet, but a sustainable way of eating that helps keep extra weight off and supports overall health. Choosing foods rich in nutrients—but not high in empty calories—supports blood sugar control and lowers the risk of complications.
Tips for Healthy Eating
- Fill half your plate with vegetables, one-quarter with lean protein, and one-quarter with whole grains; add a small portion of fruit.
- Eat a wide variety of foods to get vitamins, minerals, protein, and fiber.
- Choose nutrient-rich foods you enjoy (beans, lentils, whole-grain pasta, yogurt alternatives if lactose intolerant).
- Limit sugary drinks, sweets, and heavily processed foods.
- Watch portion sizes and read food labels.
- Track your weight and progress regularly and adjust as needed.
What to Eat with Type 2 Diabetes
Carbohydrates do not cause diabetes. Rather, the buildup of fat inside muscle cells contributes to insulin resistance, which is the root of type 2 diabetes. Diets that only focus on lowering carbohydrate intake don’t address this underlying problem—they simply compensate for the fact that insulin is not working well. By contrast, diets that reduce fat inside muscle cells can improve or even reverse insulin resistance.
Studies have shown that a whole-food, plant-based (healthy vegan) diet decreases insulin resistance and can reverse type 2 diabetes, often performing better than the standard American Diabetes Association (ADA) diet.
Resources:
- Barnard, N. D., Cohen, J., Jenkins, D. J., Turner-McGrievy, G., Gloede, L., Green, A., & Ferdowsian, H. (2009). A low-fat vegan diet and a conventional diabetes diet in the treatment of type 2 diabetes: a randomized, controlled, 74-wk clinical trial. The American journal of clinical nutrition, 89(5), 1588S–1596S. https://doi.org/10.3945/ajcn.2009.26736H Videos: If you have Prediabetes or Type 2 Diabetes, the following videos will show you how easy it is to get started with a healthier way of eating - and how surprisingly powerful it can be for your health. Please watch them in order.
- Videos:
- Further Reading
- Mastering Diabetes (Cyrus Khambatta, PhD, and Robby Barbaro, MPH)
- Dr. Neal Barnard’s Program for Reversing Diabetes
Important: If you are taking diabetes medications, talk with your primary care doctor or make an appointment in the GW Lifestyle Medicine Clinic before making major dietary changes, since your medicines may need to be adjusted as your blood sugar improves.
Evidence-Based Eating Patterns
- Whole Food Plant-Predominant Diet: A whole food plant-predominant (vegan) diet improved blood sugar and cholesterol more than standard dietary recommendations from the American Diabetes Association. [Barnard et al., 2009†doi]
- Mediterranean Diet: Research shows that following a Mediterranean-style diet—rich in vegetables, fruits, legumes, nuts, whole grains, and extra-virgin olive oil—can lower the risk of developing type 2 diabetes by about 20%. It also reduces inflammation, improves antioxidant levels, and enhances the body’s natural GLP-1 hormone to help insulin work more effectively. [Martín-Peláez et al., 2020†doi]
- Low-Carbohydrate or Ketogenic Diets: Studies suggest that a low-carbohydrate or ketogenic eating pattern can reduce A1C, improve cholesterol and triglyceride levels, and in some cases reduce the need for diabetes medications. These diets restrict sugars and refined carbohydrates while emphasizing proteins, non-starchy vegetables, and healthy fats like olive oil. [Dashti et al., 2021†doi] This dietary pattern has not been found to be sustainable in the long term and can worsen cholesterol levels and other chronic diseases. We do not recommend this dietary pattern for most patients.
- Balanced Approach: While different eating patterns (Mediterranean, low-carb, plant-based) can all be effective, the best diet is one you can sustain, that helps with weight management, and that improves your blood sugar and overall health.
Sources:
- Barnard, N. D., Cohen, J., Jenkins, D. J., Turner-McGrievy, G., Gloede, L., Green, A., & Ferdowsian, H. (2009). A low-fat vegan diet and a conventional diabetes diet in the treatment of type 2 diabetes: a randomized, controlled, 74-wk clinical trial. The American journal of clinical nutrition, 89(5), 1588S–1596S. https://doi.org/10.3945/ajcn.2009.26736H
- Martín-Peláez S, Fito M, Castaner O. Mediterranean Diet Effects on Type 2 Diabetes Prevention, Disease Progression, and Related Mechanisms. A Review. Nutrients. 2020 Jul 27;12(8):2236. doi: 10.3390/nu12082236. PMID: 32726990; PMCID: PMC7468821.
- Dashti HM, Mathew TC, Al-Zaid NS. Efficacy of Low-Carbohydrate Ketogenic Diet in the Treatment of Type 2 Diabetes. Med Princ Pract. 2021;30(3):223-235. doi: 10.1159/000512142. Epub 2020 Oct 9. PMID: 33040057; PMCID: PMC8280429.
Decrease or Eliminate Saturated Fat to Reverse Insulin Resistance
One of the main drivers of insulin resistance is dietary saturated fat. Eliminating it from the diet has been shown to reduce or reverse insulin resistance.
Saturated fats are named because of their chemical structure and are unique in that they are most often solid at room temperature. Foods with very high levels of saturated fats include butter, palm and coconut oil, cheese, and red meat.
In the typical western diet, the largest sources of saturated fat intake are from:
#1 Meat: Beef, pork and lamb contain the most saturated fat, but Americans get the most saturated fat from chicken and turkey because they eat so much of it.
#2 Dairy: Notably full-fat dairy products such as cheese.
#3 Ultra-Processed foods: These include cookies, cakes, crackers that contain significant additives and saturated fats such as butter
Vegan processed foods are also high in saturated fats due to palm and coconut oil and should be avoided.
You can find resources to support a plant predominant eating pattern at:
Lifestyle Medicine: Healthy Eating | GW Medical Faculty Associates
Foods to Choose Often
- Vegetables: leafy greens, broccoli, peppers, carrots, cucumbers
- Fruits: berries, apples, pears, citrus (in moderate portions)
- Whole grains: brown rice, quinoa, oats, whole-wheat bread or pasta
- Legumes: beans, lentils, chickpeas
- Proteins: plant-based options are optimal, free of saturated fats
- Healthy fats: nuts, seeds, avocado, olive oil, canola oil
- Dairy/alternatives: unsweetened non-fat yogurt, fortified soy or almond milk
Foods to Limit or Avoid
- Sugary drinks (soda, sweetened juices, energy drinks)
- Refined carbs (white bread, pastries, white rice, sugary cereals)
- Fried and fast foods
- Processed meats (bacon, sausage, deli meats)
- High-fat dairy (cream, whole milk, large amounts of cheese)
- Sweets and desserts (cakes, cookies, candy, ice cream)
- Packaged snacks high in salt, sugar, or saturated fat
- Protein sources high in saturated fats (beef, pork, lamb, chicken)
Takeaway: Healthy eating is about long-term habits, not short-term diets. Small, consistent changes can make a big difference in blood sugar, weight, and overall well-being.
Interactive Nutrition Facts Label
GW Lifestyle Medicine Resources on healthy eating
Clinician Notes
Mediterranean diet:
Associated with ~20% reduced risk of developing type 2 diabetes
Improves GLP-1 secretion, reduces inflammation, and raises antioxidant levels.
Low-carbohydrate/ketogenic diets:
Shown to reduce A1C, improve triglycerides and HDL, and lower medication needs in type 2 diabetes.
Plant-based diets:
Associated with improved weight control, insulin sensitivity, reduced diabetes incidence, decreased chronic kidney disease, cardiovascular disease, dementia and some cancers
Weight loss:
Losing 5–10% of body weight improves insulin sensitivity and glycemic control.
Plate method:
Practical patient tool: ½ vegetables, ¼ lean protein, ¼ whole grains, plus 1 serving of fruit.
- American Diabetes Association Professional Practice Committee; 5. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes—2025. Diabetes Care 1 January 2025; 48 (Supplement_1): S86–S127. https://doi.org/10.2337/dc25-S005
- Martín-Peláez S, Fito M, Castaner O. Mediterranean Diet Effects on Type 2 Diabetes Prevention, Disease Progression, and Related Mechanisms. A Review. Nutrients. 2020 Jul 27;12(8):2236. doi: 10.3390/nu12082236. PMID: 32726990; PMCID: PMC7468821.
- Dashti HM, Mathew TC, Al-Zaid NS. Efficacy of Low-Carbohydrate Ketogenic Diet in the Treatment of Type 2 Diabetes. Med Princ Pract. 2021;30(3):223-235. doi: 10.1159/000512142. Epub 2020 Oct 9. PMID: 33040057; PMCID: PMC8280429.
- https://www.cdc.gov/healthy-weight-growth/healthy-eating/index.html
- https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetes-diet/art-20044295
- https://www.myplate.gov/
Exercise and Diabetes
Staying active is one of the most effective ways to manage diabetes and protect your overall health. Regular exercise helps lower blood sugar, makes your body more sensitive to insulin, and reduces the risk of heart disease. It also supports weight control, improves energy, and boosts mood and well-being. Research shows that combining aerobic and resistance exercise lowers A1C more effectively than aerobic exercise alone, and that just 12 to 20 weeks of regular activity can improve insulin sensitivity in the liver. Since muscle manages your blood sugar, building more muscle through strength or resistance training helps lower blood sugar.
- Boulé NG, Kenny GP, Haddad E, Wells GA, Sigal RJ. Meta-analysis of the effect of structured exercise training on cardiorespiratory fitness in Type 2 diabetes mellitus. Diabetologia. 2003 Aug;46(8):1071-81. doi: 10.1007/s00125-003-1160-2. Epub 2003 Jul 10. PMID: 12856082.
- Kirwan JP, Sacks J, Nieuwoudt S. The essential role of exercise in the management of type 2 diabetes. Cleve Clin J Med. 2017 Jul;84(7 Suppl 1):S15-S21. doi: 10.3949/ccjm.84.s1.03. PMID: 28708479; PMCID: PMC5846677.
How Much Exercise Do I Need?
The American Diabetes Association recommends at least 150 minutes per week of moderate activity such as brisk walking, cycling, or swimming. Try to time this exercise after a meal to prevent blood sugar spikes.
- Spread this across at least 3 days per week, with no more than 2 days in a row without activity.
- Add strength training 2–3 times per week (weights, resistance bands, or body-weight exercises) to build muscle and help with daily activities.
- For older adults, balance and flexibility activities like yoga or tai chi can lower the risk of falls.
Every Bit Counts
You don’t need a gym to see results. Everyday activities—walking the dog, gardening, dancing, or taking the stairs—can help control blood sugar. Try not to sit still for long periods; standing up or walking for a few minutes every 30 minutes makes a difference.
Tips for Getting Started
- Begin slowly if you’re new to exercise and increase gradually.
- Choose activities you enjoy so it feels easier to keep up.
- Talk with your health care provider before starting vigorous exercise, especially if you have other health conditions.
GW Lifestyle Medicine Physical Activity Resources
Clinician Notes:
ADA 2025: ≥150 min/week moderate-to-vigorous aerobic activity, spread over ≥3 days/week, with no >2 days of inactivity.
Resistance training: Recommended 2–3 times/week; improves insulin sensitivity and glucose uptake.
Breaking up sedentary time: Moving every 30 min improves glycemic control (Colberg et al., ADA position statement, 2016).
Efficacy data
- Aerobic + resistance exercise reduces A1C more effectively than aerobic alone (Kirwan et al., 2017).
- 12-week aerobic training improves hepatic insulin sensitivity and reduces hepatic glucose production (Kirwan et al., 2017).
- HIIT (8 weeks) improves beta-cell function in T2D patients (Cleveland Clinic review).
- Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, Horton ES, Castorino K, Tate DF. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes care. 2016 Oct 11;39(11):2065.
- Kirwan JP, Sacks J, Nieuwoudt S. The essential role of exercise in the management of type 2 diabetes. Cleveland Clinic journal of medicine. 2017 Jul;84(7 Suppl 1):S15.
- Kanaley JA, Colberg SR, Corcoran MH, Malin SK, Rodriguez NR, Crespo CJ, Kirwan JP, Zierath JR. Exercise/physical activity in individuals with type 2 diabetes: a consensus statement from the American College of Sports Medicine. Medicine and science in sports and exercise. 2022 Feb 1;54(2):353.
- https://www.cdc.gov/physical-activity-basics/about/index.html
Resources:
- 3 steps to build healthy habits
- Why being active is important and some tips!
- Undertanding Your blood glucose and Excercise! Avoid Hypoglycemia!
- Tips for exercise and diabetes
Sleep and Diabetes
Getting enough good-quality sleep is just as important as eating well and staying active when it comes to managing diabetes. Poor sleep makes it harder for your body to use insulin, leading to higher blood sugar, weight gain, and more difficulty managing diabetes.
- Sondrup N, Termannsen AD, Eriksen JN, Hjorth MF, Færch K, Klingenberg L, Quist JS. Effects of sleep manipulation on markers of insulin sensitivity: A systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev. 2022 Apr;62:101594. doi: 10.1016/j.smrv.2022.101594. Epub 2022 Feb 1. PMID: 35189549.
- Zuraikat FM, Laferrère B, Cheng B, Scaccia SE, Cui Z, Aggarwal B, Jelic S, St-Onge MP. Chronic Insufficient Sleep in Women Impairs Insulin Sensitivity Independent of Adiposity Changes: Results of a Randomized Trial. Diabetes Care. 2024 Jan 1;47(1):117-125. doi: 10.2337/dc23-1156. PMID: 37955852; PMCID: PMC10733650.
People with diabetes are also more likely to have sleep problems such as insomnia, restless legs, or obstructive sleep apnea (OSA)—a condition where breathing repeatedly stops during sleep. Studies suggest that up to 80% of people with type 2 diabetes may have OSA, and this is linked to higher A1C, greater risk of complications, and lower quality of life.
- Foster GD, Sanders MH, Millman R, Zammit G, Borradaile KE, Newman AB, Wadden TA, Kelley D, Wing RR, Sunyer FX, Darcey V, Kuna ST; Sleep AHEAD Research Group. Obstructive sleep apnea among obese patients with type 2 diabetes. Diabetes Care. 2009 Jun;32(6):1017-9. doi: 10.2337/dc08-1776. Epub 2009 Mar 11. PMID: 19279303; PMCID: PMC2681024.
- Ogilvie RP, Patel SR. The Epidemiology of Sleep and Diabetes. Curr Diab Rep. 2018 Aug 17;18(10):82. doi: 10.1007/s11892-018-1055-8. PMID: 30120578; PMCID: PMC6437687.
The good news is that improving sleep makes a real difference. CPAP treatment for sleep apnea has been shown to lower A1C by about 0.2–0.3% and improve heart health.
- Sondrup N, Termannsen AD, Eriksen JN, Hjorth MF, Færch K, Klingenberg L, Quist JS. Effects of sleep manipulation on markers of insulin sensitivity: A systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev. 2022 Apr;62:101594. doi: 10.1016/j.smrv.2022.101594. Epub 2022 Feb 1. PMID: 35189549.
- Herth J, Sievi NA, Schmidt F, Kohler M. Effects of continuous positive airway pressure therapy on glucose metabolism in patients with obstructive sleep apnoea and type 2 diabetes: a systematic review and meta-analysis. European Respiratory Review. 2023 Sep 6;32(169).
Cognitive behavioral therapy for insomnia (CBT-I) has been proven to improve sleep and may also slightly improve blood sugar and mood. Even simple “sleep hygiene” habits—like keeping a regular bedtime, avoiding caffeine or screens late at night, and creating a dark, quiet bedroom—have been shown to improve sleep quality and even reduce A1C.
Most adults should aim for 7–9 hours of restful sleep each night. If you often feel tired, snore heavily, or wake up gasping for air, talk with your health care provider about possible sleep apnea. Addressing sleep problems can improve blood sugar, lower complication risk, and leave you feeling more energetic and focused during the day.
GW Lifestyle Medicine Sleep Resources
Clinician Notes
- Prevalence: 24–86% of people with T2D have OSA; 30–50% report insomnia; 8–45% have restless leg syndrome.
- Clinical impact: Poor sleep quality is linked to higher A1C, insulin resistance, and increased complications.
- OSA treatment: CPAP reduces A1C by ~0.24% and improves vascular health.
- Behavioral therapy: CBT-I improves sleep outcomes and may lower A1C and fasting glucose.
- Sleep hygiene: Regular bedtime, limited caffeine/electronics, quiet/dark environment improves glycemic outcomes.
- Care D. Standards of care in diabetes—2023. Diabetes care. 2023;46:S1-267.
- Henson J, Covenant A, Hall AP, Herring L, Rowlands AV, Yates T, Davies MJ. Waking up to the importance of sleep in type 2 diabetes management: a narrative review. Diabetes Care. 2024 Mar 1;47(3):331-43.
- Sondrup N, Termannsen AD, Eriksen JN, Hjorth MF, Færch K, Klingenberg L, Quist JS. Effects of sleep manipulation on markers of insulin sensitivity: A systematic review and meta-analysis of randomized controlled trials. Sleep medicine reviews. 2022 Apr 1;62:101594.
- https://www.mayoclinic.org/diseases-conditions/diabetes/symptoms-causes/syc-20371444
Relationships and Diabetes
Strong relationships and social connections are a powerful part of living well with diabetes. Having supportive family, friends, or community makes it easier to stick with healthy habits like eating well, exercising, and taking medications. Support can also lower stress and boost mood, which both play a role in blood sugar control.
On the other hand, loneliness and social isolation are linked to worse blood sugar control, higher risk of complications, and even shorter life expectancy. Studies show that people with strong social networks are more likely to have better health outcomes and a higher quality of life.
The good news is that building connections doesn’t have to be complicated. Joining a social group, attending religious or cultural activities, volunteering, or simply spending more time with loved ones can improve both emotional and physical health. Even small steps toward connecting with others can make a real difference.
Clinician Notes
- Social connection & health: Meta-analysis shows strong social relationships are associated with a 50% increased likelihood of survival.
- Loneliness & diabetes: Linked to higher A1C, poorer self-management, and more complications.
- Mechanisms: Social support reduces stress, encourages adherence to treatment, and improves resilience.
- Lifestyle Medicine: “Social connection” is one of the six recognized pillars (ACLM).
- Care D. Standards of care in diabetes—2023. Diabetes care. 2023;46:S1-267.
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS medicine. 2010 Jul 27;7(7):e1000316.
- Murthy V. Work and the loneliness epidemic. Harvard Business Review. 2017 Sep 26;9(3).
- https://lifestylemedicine.org/pillar-updates-stress-management-and-social-connection/
Stress Management and Diabetes
Stress is a normal part of life, but when it builds up it can make managing diabetes more difficult. Stress hormones like cortisol raise blood sugar and make the body less sensitive to insulin. Stress can also lead to unhealthy habits—such as overeating, skipping exercise, or forgetting medications—that worsen diabetes control.
Research shows that people with diabetes who experience high stress or “diabetes distress” often have higher A1C levels and more difficulty following their treatment plan. The good news is that healthy stress management techniques can lower stress and improve both mood and blood sugar.
- Fisher L, Glasgow RE, Strycker LA. The relationship between diabetes distress and clinical depression with glycemic control among patients with type 2 diabetes. Diabetes Care. 2010 May;33(5):1034-6. doi: 10.2337/dc09-2175. Epub 2010 Feb 11. PMID: 20150291; PMCID: PMC2858170.
- American Diabetes Association Professional Practice Committee; 5. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes—2025. Diabetes Care 1 January 2025; 48 (Supplement_1): S86–S127. https://doi.org/10.2337/dc25-S005
Simple strategies such as deep breathing, meditation, yoga, prayer, journaling, or spending time outdoors have all been shown to reduce stress. Regular physical activity is also one of the best ways to lower stress while helping to control blood sugar. Even a few minutes of relaxation each day can make a difference.
Clinician Notes
- Physiologic effects: Stress raises cortisol → ↑ blood glucose + ↓ insulin sensitivity (Mayo Clinic, 2023).
- Diabetes distress: Distinct from depression; strongly linked with higher A1C and poor adherence (Fisher et al., 2010).
- Interventions: Stress reduction programs improve coping, quality of life, and sometimes glycemic control (ADA 2025).
- Mind-body practices (yoga, mindfulness, meditation) associated with lower A1C and reduced diabetes distress in trials.
- Physical activity doubles as stress relief and glycemic management.
- Care D. Standards of care in diabetes—2023. Diabetes care. 2023;46:S1-267.
- https://health.clevelandclinic.org/stress-and-diabetes
- https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response
Drugs, Alcohol, and Diabetes
Alcohol and recreational drugs can make managing diabetes more complicated. Alcohol affects how the liver works: when your liver is busy processing alcohol, it cannot release stored glucose into the bloodstream as easily. This increases the risk of low blood sugar (hypoglycemia), especially if you take insulin or certain diabetes pills. The effects can last for hours after drinking, and because the symptoms of low blood sugar (confusion, slurred speech, unsteady walking) are similar to being drunk, it may be difficult to recognize the danger.
Alcohol can cause both high and low blood sugar and increase diabetes complications; if used, it should be rare and minimal.
- American Diabetes Association Professional Practice Committee; 5. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes—2025. Diabetes Care 1 January 2025; 48 (Supplement_1): S86–S127. https://doi.org/10.2337/dc25-S005.
Drinks also vary in carbohydrate content—beer, sweet wines, and mixed drinks can raise blood sugar, while spirits and dry wine have little carbohydrate.
Recreational drugs (such as marijuana, stimulants, or opioids) can also interfere with judgment, appetite, and medication routines, making blood sugar control unpredictable.
If you choose to drink alcohol, it’s safest to do so with food, in moderation, and never on an empty stomach. Always carry treatment for low blood sugar and let friends or family know how to help if needed. If you struggle with alcohol or drug use, talk with your health care provider—there are safe and effective resources to support you.

Clinician Notes
Alcohol & hypoglycemia:
Alcohol metabolism inhibits hepatic gluconeogenesis → ↑ risk of delayed hypoglycemia.
Moderate use:
Defined as ≤1 drink/day (women) or ≤2/day (men). Moderate intake may improve insulin sensitivity, but heavy drinking worsens glycemia and complications.
Carbohydrate content:
Beer, sweet wines, and mixed drinks can raise blood sugar, while spirits and dry wines have little to no carbohydrate and are less likely to affect glucose
Substance use disorders:
Recreational drugs disrupt self-management, increase acute risks, and worsen long-term outcomes.
Counseling:
Screen for alcohol and drug use; provide harm reduction strategies.
Summary of Healthy Habits for Diabetes
|
Healthy Habit |
What to Aim For |
Why It Helps |
| Lose a little weight | Try to lose 5–10% of your body weight if you are overweight | Even a small amount of weight loss makes your body use insulin better and lowers blood sugar. Some people can even put diabetes into remission. |
| Eat smart | Avoid Saturated fat. Fill half your plate with vegetables, add lean protein (preferably plant-based), and choose whole grains; cut back on sugary drinks and processed foods | A balanced plant-predominant diet keeps blood sugar steady, helps with weight, and protects your heart and kidneys. |
| Be active | Move at least 30 minutes a day, 5 days a week (brisk walking, biking, swimming, dancing) | Exercise lowers blood sugar, helps insulin work better, and gives you more energy. |
| Build muscle | Do strength exercises 2–3 times per week (weights, resistance bands, body-weight exercises) | Strong muscles soak up more sugar from your blood and help keep glucose levels stable. |
| Get good sleep | Aim for 7–9 hours of restful sleep each night | Poor sleep makes blood sugar harder to control and increases hunger and cravings. |
| Manage stress | Try relaxation, meditation, prayer, yoga, or spending time outdoors | Stress hormones can raise blood sugar; calming activities lower them. |
| Stay connected | Lean on family, friends, or community for support | Support makes it easier to stick with healthy habits and feel less overwhelmed. |
| Drink safely | If you drink alcohol, limit to 1 drink/day (women) or 2/day (men), and always with food | Too much alcohol can make blood sugar drop or rise unpredictably. |
| Quit smoking | Stop tobacco completely | Smoking makes diabetes harder to control and raises your risk of heart and lung problems. |
